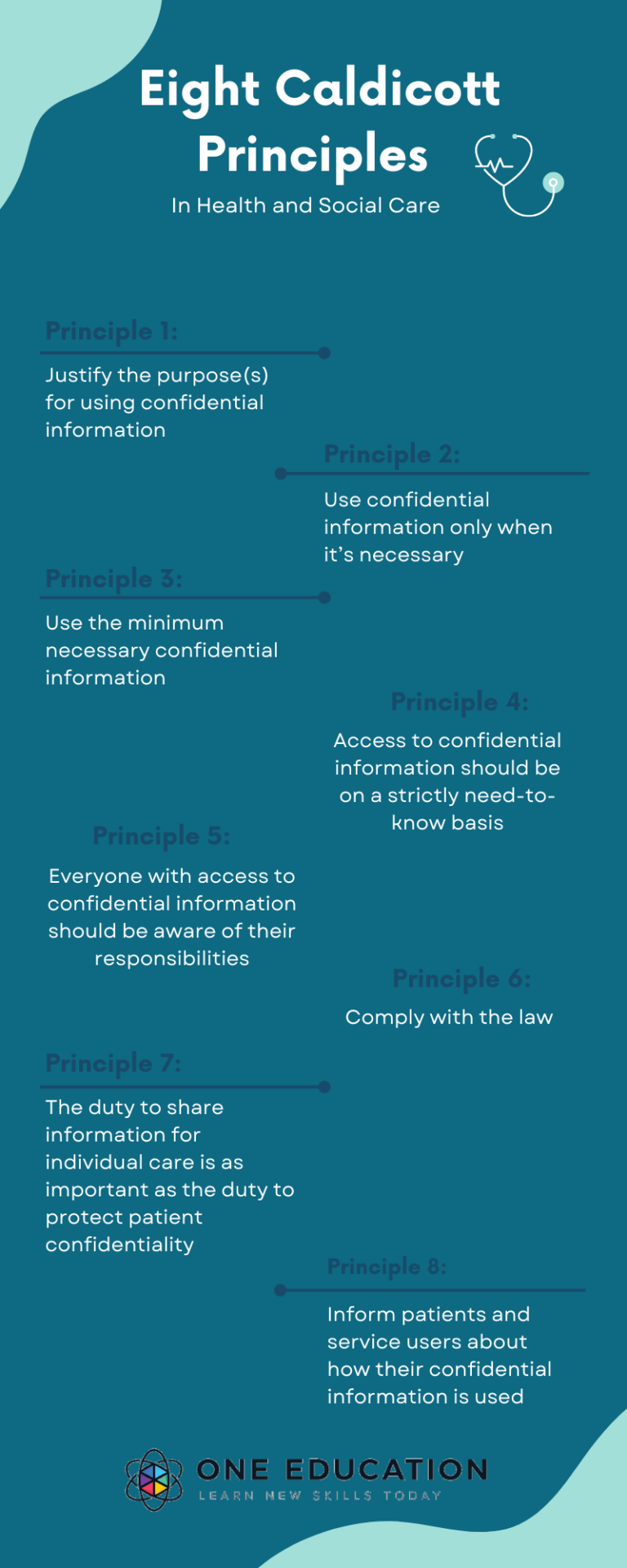
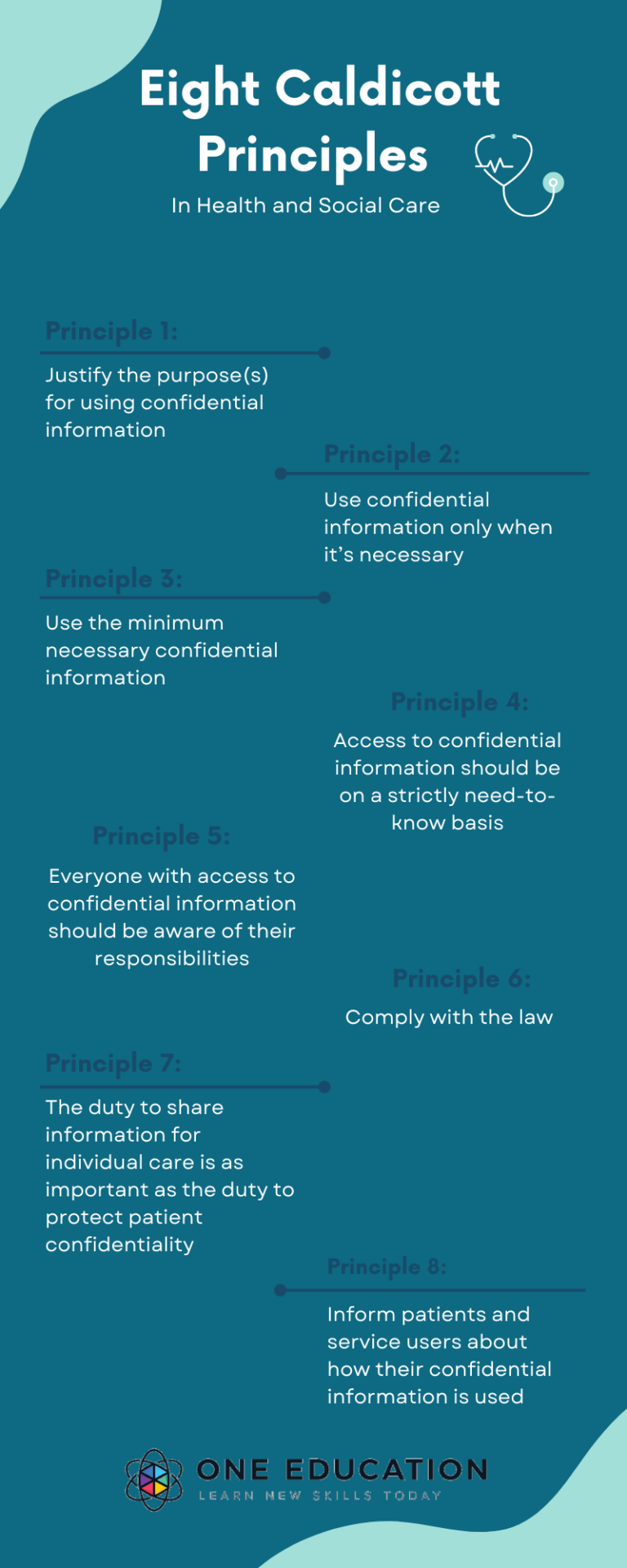
Principle 8: Inform Patients and Service Users about How Their Confidential Information is Used
The eighth Caldicott Principle states that necessary steps should be taken to ensure there are no surprises for patients and service users, and they are well-informed. They should have a clear idea about how and why their personal information will be used and their choices about this.
These steps may vary depending on the usage. As a minimum, this will include providing accessible, relevant, and appropriate information, and in some cases, greater engagement might be required.
It is important to ensure that it is done by following these principles and not outside what the policies provide. In addition, they must oversee the flow of patient information, either for research or disclosure of information to the police.

The Caldicott Principles must be followed by all health organisations, including public and private hospitals, clinics, and health or social care institutions. These principles serve as an ethical basis for staff to handle data and follow best practices.
How can You Apply Caldicott Principles in Your Settings?
Caldicott Principles must be followed by all the social and healthcare personnel to ensure that there’s no breach of confidentiality.
But some people might still be confused about whether to share information about patients in certain situations. For instance, principle 7 states, ‘The duty to share personal information can be as important as the duty to have regard for patient confidentiality.’
However, principle 7 doesn’t give a clear boundary regarding when it’s okay to share information. Instead, it merely denotes that while protecting patients’ confidentiality is necessary, there are also exceptions in the case of a breach of duty of care. So when can you share confidential information? Find out in the section below.
Here is the Caldicott Principles’ mnemonic, a reminder of Dame Fiona Caldicott herself to help you remember the Caldicott Principles.
FIONA C
- Formal justification of purpose.
- Information is to be transferred only when absolutely necessary.
- Only the minimum is required.
- Need to know access controls.
- All to understand their responsibilities.
- Comply with and understand the law.
Hopefully, this will help you remember to concentrate on patient confidentiality in your healthcare work.
When can You Share Confidential Information?
To eliminate any room for confusion, here are some situations when you should share information about a patient.
- The patient is being shifted to another hospital for treatment.
- Someone is or might be at risk of harm and needs protection.
- They are at risk of harming someone else.
- A crime might be prevented if the information is shared.
- A patient is dead, but a relative needs to be identified.
- The court or any other legal authority has requested the information.
- A serious crime has been committed, or a patient is wanted for a crime committed.
- Lastly, when the law authorises it.
However, any member of the Executive, such as the police, does not have the right to request patient-identifiable information without a written order by the court. If there is a written order, but the information is still being withheld, the patient’s doctor could be held in contempt of court.
Who is a Caldicott Guardian?
A Caldicott Guardian is a person responsible for preserving the confidentiality of people’s health and care information. And the Caldicott Guardian is usually a board-level health professional or deputy.
Therefore, the Caldicott Guardian should be as follows, in order of priority –
- A member of the management board or senior management team of the health or social care organisation.
- A senior health or social care professional.
- A member of staff who has the responsibility for promoting clinical governance or equivalent in the organisation.
All NHS organisations and local authorities that provide social services need to have a Caldicott Guardian. The national body for Caldicott Guardians is the UK Caldicott Guardian Council (UKCGC).
The Role of a Caldicott Guardian
A Caldicott Guardian’s key responsibilities include championing confidentiality at the senior management level, internal information processing and information. But most importantly, they have excellent knowledge and expertise in confidentiality and data protection.
Caldicott Guardians are responsible for developing local protocols for information disclosure, restricting access to patient information by enforcing strict need-to-know principles, and regularly reviewing and justifying patient information use. In addition, Caldicott Guardians make sure that patient-identifiable information are used legally, ethically and appropriately.
The role of the Caldicott Guardian for both health and social care covers the wider aspects of information management, including the following laws:
- Data Protection Act 2018
- NHS Act 2006 (section 251)
- Freedom of Information Act 2000
- Human Rights Act 1998
- Computer Misuse Act 1990
- NHS Constitution (January 2009, updated February 2015)
- NHS Information Governance
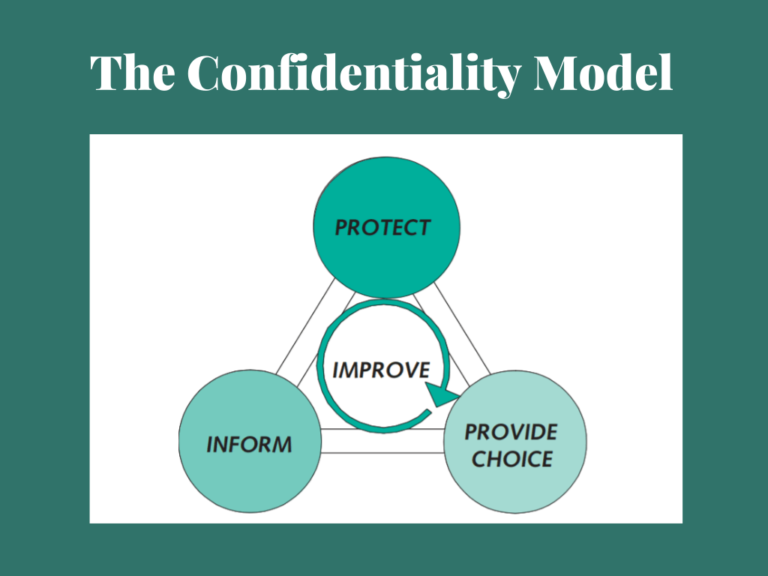
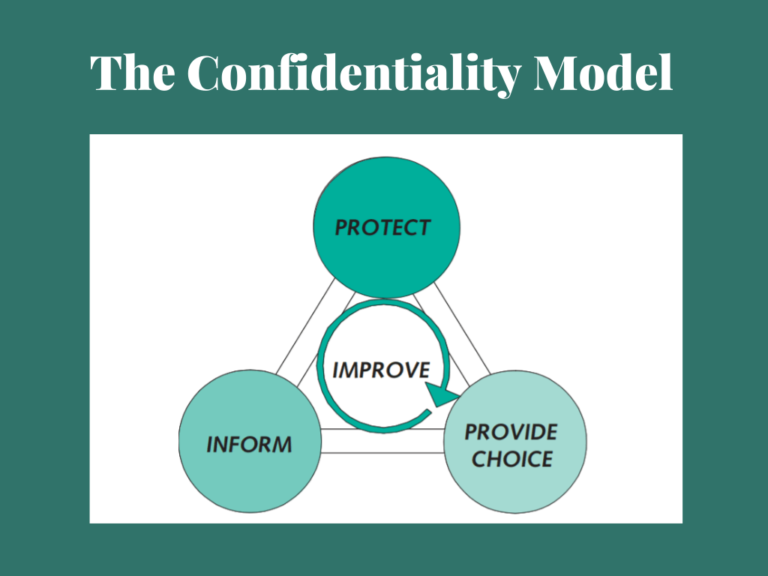
The following confidentiality model used by the NHS and Caldicott Guardian’s is also very beneficial in protecting patients’ confidentiality.
A Caldicott Guardian must approve of it before sharing information. And there is a Caldicott Guardian appointed to each hospital to ensure that every member of social and health care staff follows the Caldicott Principles. And the guardian reviews the procedures relating to person-identifiable health data and safeguards patients.
The guardian should also have a close relationship with the senior health professional responsible for promoting clinical governance or the equivalent of social care.
Download Free Poster of 8 Caldicott Principles


![]() 18 minutes
18 minutes